I wrote this page after many trans women planning to get bottom surgery told me they had no idea what a vulva looked like. They basically had no idea what to say to the surgeon to express concerns. One friend wrote about her labiaplasty:
As they prepared to give me the general, and Dr. Schrang walked into the OR, he asked me if I had any special requests, to which I responded quite truthfully, “Uh, I don’t know.” He then asked me if my clitoris was too large, and I kind of stared at him, and answered, “I have no idea.” It was very amusing, and I think the anesthesiologist was having to bite his tongue to keep from laughing.
Luckily, she trusted the surgeon to make everything look right, but it would have been better if she had common points of reference for a discussion of cosmetic and functional outcomes. I very surprised how badly my friends wanted vaginoplasty, but really didn’t know what exactly it was they wanted. It seems to me that they were more interested in not having a penis than in what they’d end up with.
Turns out it’s not just younger trans women, either. The day after I put up this page, a friend who is older than I am sent me this note:
You can add me to the group who had no idea what I would end up with, I just knew it was a lot better than what I had. I will be quite honest with you here, please don’t post this with my name or spread knowledge of my ignorance around. I had very little idea of what I would end up with. I knew I would have Labia and a vaginal cavity, but I had no idea what the urethra was or where it would be located. I knew very little about the clitoris or its position or function. The mons pubis was a total mystery to me until I bumped it too hard!
I feel that awareness and understanding of your genitalia is fundamental to ownership and control of your own body. Not just in a sexual sense, either. You need to be aware of all the parts and attendant joys and difficulties.
Keep in mind that while genital anatomy is basically the same, each person is also different. Differences in size, color and shape are part of human diversity. As with penises, women’s external genitalia vary quite significantly. If you have aesthetic or functional concerns either before or after surgery, contact your health care provider.
AMAB anatomy, side view
Most people who are assigned male at birth (AMAB) have these reproductive organs.
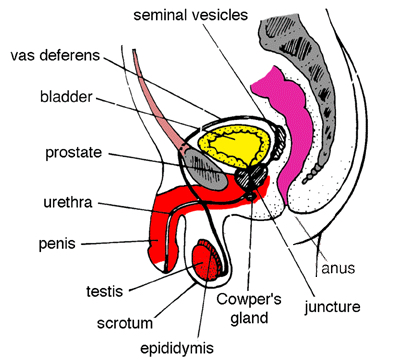
Color coding:
The organ I have colored yellow is the bladder, which holds urine. It’s right behind your pubic bone. When you have to urinate, you empty your bladder through your urethra, In most AMAB genitalia, the urethra is longer and goes through the penis and out the end. In vaginoplasty, the surgeon shortens the urethra so it’s more like the urethra in the diagram below.
The organ I have colored pink is the colon. This is where solid waste is held until you expel it from the anus. Some vaginoplasty procedures use tissue from this area.
The gray bone behind the colon is your spine. The gray bone in front of your bladder is your pubic bone. Attached to the pubic bone are your abdominal muscles.
Areas I’ve marked in red are removed during vaginoplasty. This includes the testicles or testes, where most testosterone, or more accurately, androgens, sperm, and some semen can be produced. Once the testicles are removed, your production of androgens is virtually eliminated, and you are no longer able to produce sperm. Also removed is most of the spongy erectile tissue (corpus spongiosum) inside the penis.
In most vaginoplasty procedures, the skin from the penis and scrotum is usually used for making the lining of your vagina (called the penile inversion technique), as well as for making the features of your vulva or external genitalia (discussed below).
You’ll note that I didn’t color all of the tip of the penis red. That’s because the surgeon will use part of this to make your clitoris (see below).
Now, you may think this paragraph is gross or unimportant, but you need to understand how semen is produced. Please read this! Semen is the white milky fluid that people with testicles ejaculate when they have an orgasm. Semen has only a tiny amount of sperm, which can fertilize an egg and produce a baby. The rest is a mixture of other fluids: nutrients for the sperm from the seminal vesicles, mucus from the Cowper’s gland, and an alkaline secretion from the prostate (this alkaline offsets the acids found inside the vagina, so the sperm aren’t killed as they travel into the uterus).The prostate is a gland that is at the base of the bladder. If you look at the diagram above, you’ll see that semen travels from the testes through a tube called the vas deferens. The vas deferens eventually connects with the urethra at a juncture near the prostate. When AMAB people with all these organs ejaculate (come), muscles around the prostate and other glands contract and shoot the semen and sperm out the end of the penis.
Important note:
Surgeons do not remove the prostate gland and Cowper’s gland in the current techniques.
This means you will have some secretions when aroused from these glands. This will frequently not be enough for lubrication during sex for many women, but you will have some.
Also, for this reason, it’s important to have a prostate exam whenever you have a gynecological exam. Prostate cancer is a major killer, although the likelihood in trans women is probably significantly reduced. Still, you should have it checked regularly along with your breasts and vagina, especially after 35.
AFAB anatomy, side view
Most people who are assigned female at birth (AFAB) have these reproductive organs.
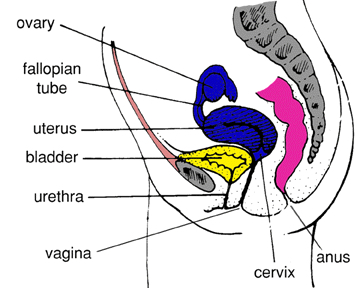
Color coding:
The organ I have colored yellow is the bladder, which holds urine. It’s right behind your pubic bone. When you have to urinate, you empty your bladder through your urethra, In AFAB genitalia, the urethra is shorter. It’s located between the clitoris and the vagina. You’ll notice there tends to be a general difference in the size and placement of the bladder is you look at both diagrams.
The organ I have colored pink is the colon. This is where solid waste is held until you expel it. One vaginoplasty procedure uses tissue from this area, but most do not.
The gray bone behind the colon is your spine. The gray bone in front of your bladder is your pubic bone. Attached to the pubic bone are your abdominal muscles. Generally, the AMAB pubic bone is a bit more prominent and larger.
Areas I’ve colored blue above and marked with asterisks(*) below are not constructed as part of current vaginoplasty techniques. They are reproductive organs in many AFAB people, for reference. They are the organs that allow egg production, ovulation, pregnancy and childbirth, menstruation, etc.
Cervix*
- The base of the uterus which extends into the vaginal canal. In its center is a small opening into the uterus, called the cervical os (mouth).
Uterus (womb)*
- The pear-shaped muscular organ situated in the pelvic cavity that receives and holds the fertilized ovum (egg). This is where it grows for about nine months until it is born.
Ovaries*
- The two small organs located on either side of the uterus, in which ova (eggs) are stored and grow to maturation. The ovaries are the structural equivalent of the testes. They are the place where sex hormones (estrogen and progesterone) are produced. That is why many cisgender women choose to take feminizing hormones after a hysterectomy. Trans women and transfeminine people often choose to take feminizing hormones orhiectomy vaginoplasty. The ovaries are also where eggs are produced.
Fallopian tubes (oviducts)*
- The two small tubes which extend from the ovaries to the uterus, through which eggs travel. About once a month, a mature egg travels down the fallopian tube (the structural equivalent of the vas deferens). If the egg is fertilized with sperm as it travels down the fallopian tube, it becomes a fetus.
Important note:
One thing I want to emphasize is that not having these reproductive organs doesn’t mean you aren’t a real woman. Many people are born without some or all of these parts, or their parts have some condition so that they are not able to have children. The ability to bear children is by no means the essence of womanhood.
As you can see, there isn’t a huge difference physiologically. Basically, the surgeon simply removes the inside of the penis and testicles, then uses the skin to make a vagina, clitoris, labia, and a shorter urethra. All of this is discussed in detail below.
AFAB anatomy, front view
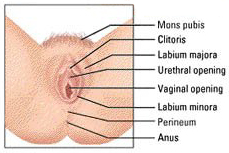
Glossary
Organs below marked with an asterisk(*) are not constructed as part of current vaginoplasty techniques.
Vulva (VUL-vuh)
- The vulva is a collective term used to describe the visible external genital organs, extending from the mons pubis to the perineum. The external genitalia consist of the clitoris and clitoral hood, and the labia majora and labia minora.
Mons pubis (Mahns PEW-bis)
- The soft fatty tissue covered with pubic hair which lies on top of the pubic bone. You have this before surgery. After surgery, your clitoris will be on the lower part of the mons pubis.
Labia majora (LAY-be-uh MUH-jo-ruh)
- Labia majora means “large lips” in Latin. The labia majora are the large, outer lips of the vulva that extend from the mons pubis down either side of the vulva. They are covered by pubic hair and contain fatty tissue under the skin. The soft folds of skin which form flaps on the outer part of the vulva. In sex-reassignment surgery, these are fashioned from scrotal tissue.
Labia minora (LAY-be-uh My-NOR-uh)
- Labia minora means “small lips” in Latin. The labia minora are the smaller, fleshy inner lips of the vulva that are inside the labia majora and closer to the vaginal opening. The folds within the labia majora which surround and cover the openings of the urethra and the vagina. They are not covered by pubic hair. The size, color, and shape of the labia minora varies a great deal. Some cisgender women even have larger inner lips than outer. These tend to be not as pronounced in trans women, especially in those who opt for a one-stage vaginoplasty with no labiaplasty follow-up.
Clitoris (CLIT-or-is)
- The clitoris is a small, firm, rounded organ at the top of the vulva within the labia majora, just above the urethra, that measures about 1/4 of an inch– that’s just about the size of a pencil eraser. The clitoris is an important organ for sexual responsiveness. It is composed of erectile tissue and blood vessels. The clitoris is formed from the head of the penis during surgery.The external part of the clitoris, called the glans, is covered by a hood of skin. It is connected to a shaft which extends upwards internally toward the pubic bone. During surgery, the same shaft of nerves that extends through the penis is used to form a shaft that you can feel around the clitoris and sometimes on the upper side of the vagina.When the clitoris is aroused, it fills with blood, becoming harder and more sensitive. The sole purpose of the clitoris is sexual sensation and if sufficiently stimulated it will produce orgasm. Many trans women focus on vaginal orgasms (stimulation caused by penetration), but for most trans women and non-trans women, it’s much easier to have an orgasm through direct clitoral stimulation with a finger, vibrator, partner’s tongue, or a partner rubbing or bumping their mons pubis against yours.Size and position of clitoris during surgery is an important aesthetic and functional consideration. While non-trans women vary greatly in clitoral size, it’s not unusual for trans women to have a larger than average clitoris. Sometimes, it’s well outside cisgender range. Most surgeons are well aware of this potential outcome and take steps to avoid it. It’s also not unusual for the clitoris to be in a slightly unusual position. This is especially true when a surgeon attempts to accommodate a patient’s request for a lot of depth.
Urethra Urethra (You-REE-thruh)
- The urethra is a short tube connected to the bladder that transports urine to the urethral opening. This opening can be seen as a very small, v-shaped dimple below the clitoris. During surgery, the surgeon removes the spongy penile tissue that surrounds the urethra and uses the urethral tube itself for your new urethra.It’s not uncommon in trans women to have a slightly more pronounced and wider urethra. It’s also fairly common for the urine stream to go in a more forward direction than in cisgender women. This might mean you have to sit back on the toilet a bit more and lean forward some. No biggie.
Vagina
- The muscular canal that leads from the vaginal opening. It is a narrow tunnel that usually measures between three and six inches in length. The vaginal opening is called the introitus, through which flows vaginal discharge. A certain degree of vaginal discharge is common, and may change in consistency depending on the hormones present . Because a constructed vagina will not have the same glandular secretions, you may experience dryness, irritation or even infection.In vaginoplasty, the vagina is formed by removing the spongy penile tissue and forming a pocket inside the body. This new pocket is then lined with skin from the penis and scrotum, which is inverted (turned inside out) and tucked into the pocket.Generally, trans women seem to have stronger muscles in the vagina. For this reason, it’s important to dilate, not just to avoid losing depth, but also width. In fact, width will probably play a greater role in comfort during penetrative sex.
Perineum (Pair-in-EE-um)
- The perineum is the area between the vagina and the anus.
Anus
- The anus is the outer opening to the rectum and bowels. After puberty, pubic hair may grow around the anus, and the skin may darken in color.
Hymen*
- The hymen is a thin, delicate mucous membrane surrounding and partially covering the vaginal opening, which becomes stretched and/or broken when a finger, tampon, penis, or other object is inserted into the vagina. Despite myths to the contrary, it is not an indication of virginity. This is not constructed during surgery.
Skene’s ducts* and Barthlolin’s glands* both are somewhat mysterious. They’re just under the skin and produce secretions believed to aid in lubrication and to ward off infection. You won’t have either of ’em, so don’t worry about ’em.
Depth
Some trans women are concerned about vaginal depth. Most non-trans women have between 3 to 6 inches of depth, which is plenty in the majority of sexual encounters with men. The largest dilator given out by most surgeons is larger than an average penis. If you can accommodate this dilator, you shouldn’t have problems accommodating most men. If you find yourself with a man who has a larger than average penis, it’s quite likely he has met non-trans women who had difficulty accommodating him as well.
Most women I know who have had the penile inversion technique with a scrotal graft have had 5 to 6 inches of depth, with one a little past 7 inches.
After surgery
Besides not knowing (or wanting to know) what their surgical outcome should look like, many trans women are squeamish about seeing what their outcome does look like. Even more are afraid to see what it feels like. Check things out every now and then– it’s very important to be aware of your body. Having hangups or being disgusted by your own body can lead to serious mental and medical problems.
The following info is largely from the wonderful U by Kotex website:
When it comes to your body, you’re the biggest expert around. After all, you live there; you know its workings best. But no matter how young or old you are, your body’s shape, hormones and capabilities are changing, in teeny, almost imperceptible ways, all the time. So you owe it to yourself to know what’s going on, inside and out.
Outer genitals
The best way to become familiar with what’s down there is the same way you learned about other parts of your body: by looking at them. However, these particular parts are rather inconveniently placed for direct staring-at-them purposes. Therefore, you might wish to consult an illustration, or better yet, use a mirror to hold between your legs. Most vaginoplasty surgeons supply a hand mirror, but if not, go buy one or use one from a compact.
That whole area you’re looking at is called the vulva, a.k.a. “external genitalia.”
At the top of the genital region, where your pubic hair begins, you’ll feel a round bone called the mons. Check out below. See the soft flaps of skin? These are the labia majora (outer lips). Inside the protective outer lips, you’ll find another, more delicate pair of lips called the labia minora (inner lips). There’s a lot of variation in appearance here: Some women’s inner lips are bigger than their outer ones, some are more wrinkled or paler or darker or whatever.
Between your inner lips, high up, is a protective fold of skin. This is called the clitoral hood. If you pull it back gently, you’ll expose a teeny, round bulge. This is your clitoris, which plays an important, positive role in a woman’s sexuality. The clitoris is rich with nerve endings and extremely sensitive.
Just below your clitoris you’ll see a small opening, the urethra. This is the opening through which you urinate. Continuing downward, below your urethra, you’ll see a larger opening, which is your vagina.
Don’t be squeamish about touching everything. It’s really important to feel around and get a sense of what you have. A good place to feel around can be in the shower when you’re washing the area.
Inner genitals
You should also put your fingers up into your vagina to see how it feels. Do it in the shower, or on the bed just prior to dilation.
Use a little lubrication. I can tell you from experience that it feels just like the inside of a non-trans woman’s vagina.
Also, I recommend checking out my page on dilation for more information on care and maintenance.
Similarities to non-trans genitalia
In 2001, a reader sent along this good news after she and her cis woman partner did some careful exploring of each other:
My partner and I ordered some toys from a wonderful shop in Seattle, and I noticed that for six dollars I could pick up a speculum. With the help of a pen light and a hand mirror, we explored one another and I made the most delightful discovery.
The only visible difference between our vaginas is that at the termination of hers is a tiny, round donut-shaped depression about the size of a pencil eraser (her cervix). I’d heard the results looked good to OB/GYNs anecdotally, but seeing it myself made me irrationally happy. I think I’d imagined this would look different, that perhaps scar lines would be visible or the character of the tissues would be noticeably different. That six dollars is one of my best investments to date and, as I imply, assuaged some unarticulated trepidation I had.
Resources
For an excellent published example of the variety, check out Joani Blank’s Femalia. Published by Down There Press; 32 photos; ISBN 0-940208-15-6.
A New View of a Woman’s Body by Federation of Feminist Women’s Health Center, is a great book, too.
Non trans-specific resources
Clue (helloclue.com)
Our Bodies, Ourselves (ourbodiesourselves.org)
- The Boston Women’s Health Collective is one of the finest books ever written for women– everyone should own a copy!
Advocates For Youth (advocatesforyouth.org)
- Calls for politicians to “Respect Young People’s Right To Be Responsible”. Excellent site that has a section focusing on responsible sexual rights of adolescents, with excellent reading material about sex education elsewhere in the world and how it compares to the U.S.
The Coalition For Positive Sexuality (positive.org)
- I used to work with this group when they were a scrappy little activist group fighting for sex ed in Chicago Public Schools (hence the initials CPS). Their “Just Say Yes” campaign was part of the response to the sex-negative climate during the Reagan years (and a play on their “Just Say No” campaign). They have excellent instructions on condoms and other safe sex practices.
Ask Alice! (goaskalice.columbia.edu)
- Now one of the most established and well-known resources available to people of all ages dealing with health, in general, and more specifically, sexuality and sexual health. It is run by Columbia University in New York and is very well done.
Condomania (condomania.com)
- Everything You Always Wanted To Know About Condoms!! – A Fantastic Resource From The People At CONDOMANIA!
SIECUS (siecus.org)
- The Sexuality Information Education Council of the United States – A resource geared toward sex educators and parents.